Understanding Lyme Disease in children
What is Lyme Disease?
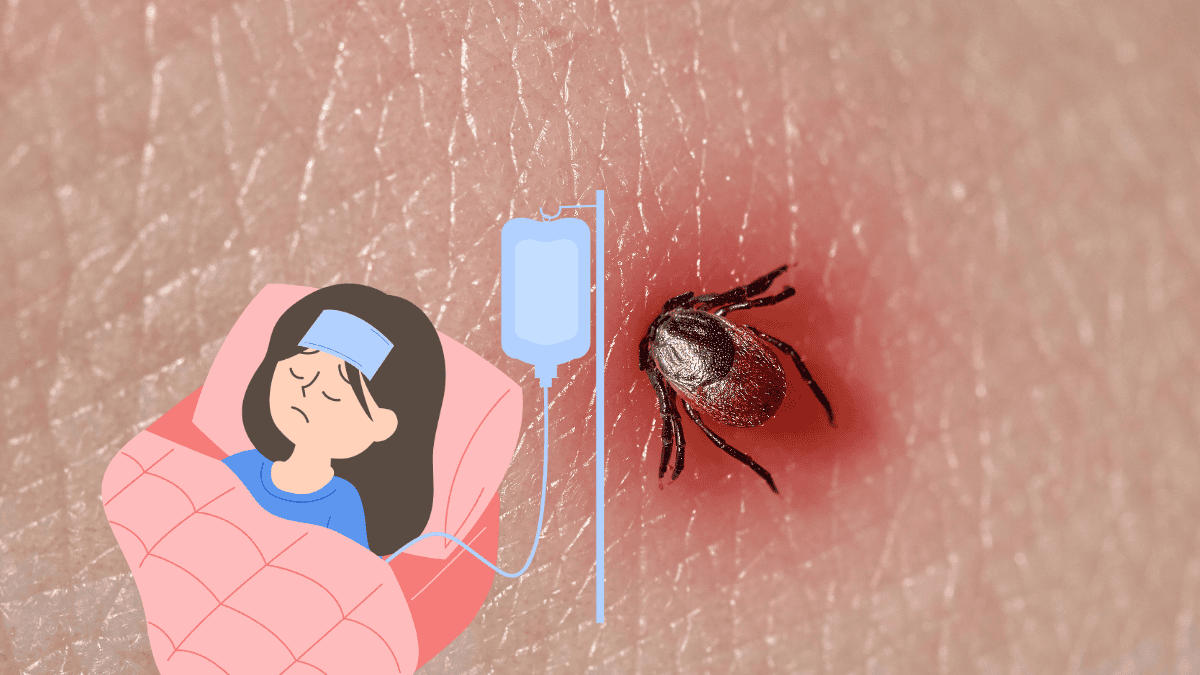
Lyme disease is an infectious illness caused by the bacterium Borrelia burgdorferi, which is transmitted to humans through the bite of infected black-legged ticks, also known as deer ticks. The disease is most commonly found in wooded and grassy areas where these ticks thrive.
Early symptoms of Lyme disease can include fever, chills, headache, fatigue, muscle and joint aches, and swollen lymph nodes. One of the hallmark signs of Lyme disease is a characteristic skin rash known as erythema migrans, which often looks like a “bull’s-eye” with a central red spot surrounded by a clear area and a red ring.
If left untreated, Lyme disease can progress to more severe symptoms affecting the heart, joints, and nervous system. Treatment usually involves antibiotics, and the disease is most effectively treated when caught early.
How Lyme Disease Affects Children
Lyme disease can impact children in a number of ways, and understanding these effects is crucial for early detection and treatment. Here are some key points on how Lyme disease affects children:
- Symptoms: In children, Lyme disease symptoms can be similar to those in adults, but they might present differently. Children may experience the classic rash, though it’s not always noticeable. They might also have flu-like symptoms, such as fever, headache, and fatigue, which can sometimes be mistaken for other illnesses. Joint pain or swelling can also be a symptom, and in some cases, children might have difficulty with coordination or experience unusual tiredness.
- Diagnosis Challenges: Diagnosing Lyme disease in children can be challenging because its symptoms can overlap with those of other common childhood illnesses. Additionally, not all children with Lyme disease develop the characteristic rash. Therefore, it’s important for parents and caregivers to be vigilant about tick bites and consult a healthcare provider if symptoms suggestive of Lyme disease develop.
- Potential Complications: If Lyme disease is not treated promptly, it can lead to complications such as Lyme arthritis, which is characterized by swelling and pain in the joints, particularly in the knees.
- Neurological complications can also occur, including Lyme neuroborreliosis, which can lead to issues such as facial paralysis or meningitis. However, these severe complications are relatively rare and typically occur when the disease is left untreated.
- Treatment: The treatment for Lyme disease in children is similar to that in adults and usually involves antibiotics. Early treatment is generally very effective, and most children recover fully without any long-term effects. However, it’s important for treatment to be administered based on a healthcare provider’s diagnosis to ensure appropriate care.
- Prevention: Preventing Lyme disease involves avoiding tick bites by using insect repellent, wearing protective clothing, and performing tick checks after spending time in tick-infested areas. Teaching children to recognize and report tick bites can also help in early removal and prevention of disease transmission.

Symptoms of Lyme Disease in Children
Early Symptoms of Lyme Disease
In children, early symptoms of Lyme disease can be subtle and sometimes mistaken for other common illnesses. Key early symptoms include:
- Fever and Chills: Often the first noticeable signs, these can mimic the flu or other infections.
- Headache: A common symptom that can range from mild to severe.
- Fatigue: Unusual tiredness or lethargy, which might affect a child’s usual activity levels.
- Muscle and Joint Aches: These can present as general discomfort or more localized pain.
- Swollen Lymph Nodes: These might be felt in areas like the neck, armpits, or groin.
- Erythema Migrans: The classic “bull’s-eye” rash may appear, though it’s not always present. The rash typically starts as a small red spot and expands over time, forming a ring around the center.
Later Symptoms and Complications
If Lyme disease progresses without treatment, more severe symptoms and complications can develop
- Lyme Arthritis: This is one of the most common complications, characterized by swelling, pain, and stiffness in the joints, often affecting the knees. Joint issues can become chronic if not treated properly.
- Neurological Issues: These can include Lyme neuroborreliosis, which may cause problems such as facial paralysis (Bell’s palsy), meningitis (inflammation of the protective membranes covering the brain and spinal cord), and cognitive difficulties.
- Cardiac Problems: Although rare, Lyme carditis can occur, leading to heart irregularities such as palpitations or even heart block.
- Fatigue and Malaise: Persistent fatigue can continue even after treatment and may affect the child’s ability to return to normal activities.
How Symptoms Differ in Children
Symptoms of Lyme disease in children can differ from those in adults in several ways:
- Difficulty Describing Symptoms: Young children might have trouble articulating their symptoms, which can make diagnosis more challenging. They might express discomfort through behavioral changes, such as irritability or changes in sleep patterns.
- Presentation of Rash: The classic “bull’s-eye” rash might be less noticeable in children or might not appear at all. Instead, the rash could be atypical or mistaken for other skin conditions.
- Behavioral Changes: Children might show changes in behavior, such as becoming unusually tired, irritable, or reluctant to engage in usual activities. This can sometimes be a key indicator for parents.
- Joint Symptoms: Joint pain or swelling in children might be more localized and less pronounced than in adults. They may not always complain of joint pain directly but might show signs of discomfort or limping.
Diagnosing Lyme Disease in Children
Common Diagnostic Tests
Diagnosing Lyme disease in children typically involves a combination of clinical evaluation and laboratory tests. Common diagnostic tests include:
- Clinical Assessment: A thorough medical history and physical examination are critical. Healthcare providers will look for symptoms like the characteristic rash (erythema migrans), fever, and joint pain, as well as inquire about recent tick exposure.
- ELISA Test: The Enzyme-Linked Immunosorbent Assay (ELISA) is a blood test used to detect antibodies against Borrelia burgdorferi. A positive result suggests exposure to the bacteria, but it is not conclusive on its own.
- Western Blot Test: This test is often used to confirm an ELISA result. It identifies specific proteins associated with the Lyme disease bacteria and helps confirm an infection.
- Polymerase Chain Reaction (PCR): PCR tests can detect Borrelia burgdorferi DNA in body fluids such as blood, cerebrospinal fluid, or joint fluid. This test is more specific but less commonly used due to its complexity and cost.
- Serology: This involves detecting antibodies in the blood. In children, serological tests may be less reliable early in the infection, as it can take several weeks for antibodies to develop.
Challenges in Diagnosing Lyme Disease in Kids
Diagnosing Lyme disease in children presents several challenges:
- Non-Specific Symptoms: Early symptoms of Lyme disease, such as fever, headache, and fatigue, are common to many other illnesses, making it difficult to pinpoint Lyme disease without further testing.
- Inconsistent Rash Presentation: Not all children with Lyme disease develop the characteristic “bull’s-eye” rash. The rash can appear atypically or be mistaken for other skin conditions.
- Difficulty Articulating Symptoms: Younger children may have trouble describing their symptoms, which can delay diagnosis. Behavioral changes might be the only clue, which can be subtle and easily overlooked.
- False Negatives: Initial tests might yield false negatives, especially if performed too early in the infection before antibodies have developed. This can lead to missed or delayed diagnosis.
- Regional Variability: Lyme disease prevalence varies by geographic location. In areas where Lyme disease is less common, physicians might be less likely to consider it as a diagnosis, potentially leading to underdiagnosis.
Treatment Options for Lyme Disease
Antibiotic Treatment
Antibiotic treatment is the primary method for managing Lyme disease and is most effective when administered early in the infection. The choice of antibiotics and the duration of treatment depend on the stage of the disease and the specific symptoms present. Commonly prescribed antibiotics include:
- Doxycycline: Often used for adults and children over 8 years old. It is usually prescribed for 10-14 days.
- Amoxicillin: An alternative for younger children or pregnant women. Typically given for 14-21 days.
- Cefuroxime axetil: Another alternative that can be used in a 14-21 day regimen.
- Intravenous Antibiotics: In cases of severe symptoms, such as neurological or cardiac involvement, intravenous antibiotics like ceftriaxone may be required for 2-4 weeks.
Antibiotics are highly effective in treating early-stage Lyme disease and can prevent the progression to more severe stages. However, it’s important to complete the full course of antibiotics as prescribed to ensure the infection is fully cleared.
conclusion
Lyme disease, caused by the bacterium Borrelia burgdorferi and transmitted through tick bites, presents a range of symptoms that can affect both adults and children. Early detection and treatment are crucial for effective management and recovery. Recognizing the early symptoms, such as fever, headache, and the characteristic rash, can facilitate prompt diagnosis and intervention.
Antibiotic treatment remains the cornerstone of managing Lyme disease, with medications like doxycycline, amoxicillin, and cefuroxime axetil being effective in treating the infection. In severe cases, intravenous antibiotics may be necessary. While conventional treatments are essential, some individuals may also explore complementary therapies to support overall health and symptom management. These should be considered as adjuncts to, rather than replacements for, prescribed antibiotics.
Diagnosing Lyme disease in children can be particularly challenging due to the non-specific nature of early symptoms and the variability in how the disease presents. Parents should be vigilant about tick exposure and seek medical advice if symptoms suggestive of Lyme disease arise.
Frequently Asked Questions (FAQs)
How common is Lyme disease in children?
Lyme disease is common in certain regions, particularly in the northeastern and north-central U.S., and in parts of Europe and Asia. Children are at higher risk due to frequent outdoor activities in tick-infested areas.
Can Lyme disease be cured completely?
Yes, Lyme disease can usually be cured completely with antibiotics, especially if treated early. Some people may experience lingering symptoms even after treatment, but most recover fully.
What should parents know about Lyme disease?
Parents should:
Know the Risks: Be aware of tick habitats and high-risk areas.
Prevent Tick Bites: Use repellent, wear protective clothing, and check for ticks.
Watch for Symptoms: Look for fever, rash, headache, and joint pain.
Seek Medical Advice: Consult a healthcare provider if symptoms or tick exposure occur.
Complete Treatment: Ensure full antibiotic courses are completed and follow up if symptoms persist.