Understanding FDA’s role in FDA fatty liver disease,
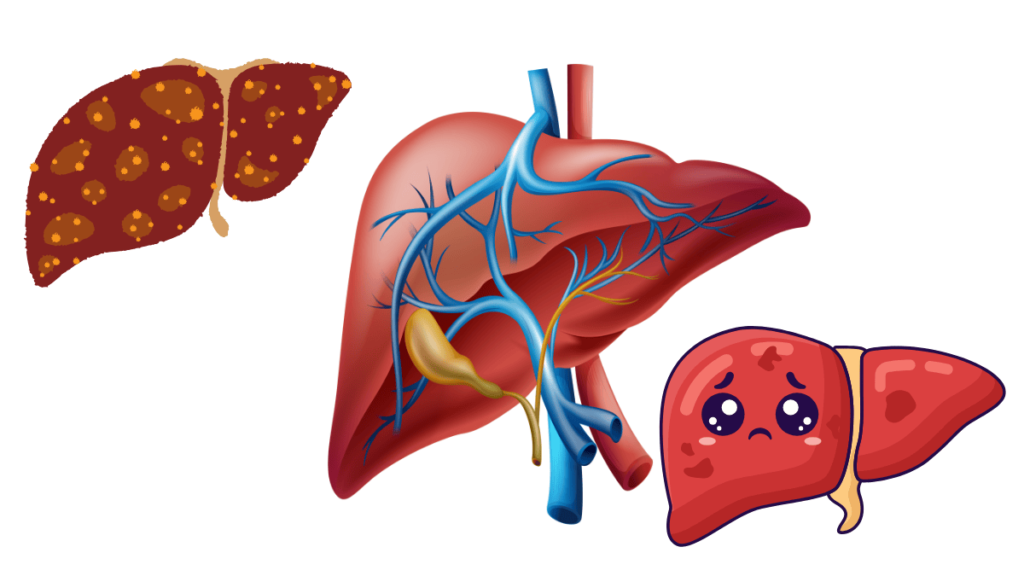
What is Fatty Liver Disease?
Adipose liver complaint is a condition where redundant fat accumulates in the liver cells. This buildup can interfere with the liver’s normal functions and may lead to inflammation, scarring, or other serious liver conditions. Fatty liver disease is often asymptomatic in its early stages, making it crucial to understand its types, causes, and risk factors to ensure early detection and effective management.
Types of Fatty Liver Disease
Fatty liver disease can be broadly categorized into two main types, each with distinct causes and implications for health.
Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-Alcoholic Fatty Liver Disease (NAFLD) is characterized by fat accumulation in the liver unrelated to alcohol consumption. It is the most common form of fatty liver disease and is often associated with metabolic conditions. NAFLD can range from simple fat accumulation (steatosis) to more severe liver damage, including inflammation and fibrosis, leading to non-alcoholic steatohepatitis (NASH).
Key Points
- Prevalence: NAFLD affects a significant portion of the global population, particularly those with obesity, diabetes, and metabolic syndrome.
- Symptoms: Many people with NAFLD experience no symptoms. When symptoms do occur, they may include fatigue, abdominal discomfort, or elevated liver enzymes.
- Diagnosis: NAFLD is typically diagnosed through imaging studies like ultrasound or MRI and confirmed with liver biopsy if necessary.
- Management: Lifestyle changes, including weight loss, healthy eating, and regular exercise, are fundamental in managing NAFLD. Medications and treatments may be prescribed in more severe cases.
Alcoholic Fatty Liver Disease (AFLD)
Alcoholic Fatty Liver Disease (AFLD) results from excessive alcohol consumption. It is the initial stage of alcohol-related liver disease and can progress to more severe conditions like alcoholic hepatitis or cirrhosis if alcohol intake is not reduced or eliminated.
Key Points
- Prevalence: AFLD is directly linked to alcohol consumption patterns. The risk increases with the amount and duration of alcohol intake.
- Symptoms: Symptoms may include abdominal pain, nausea, vomiting, and jaundice. Severe cases can lead to liver failure.
- Diagnosis: AFLD is diagnosed through patient history, physical examination, and imaging studies. Liver biopsy may be used to assess the extent of liver damage.
- Management: The primary treatment for AFLD is to cease alcohol consumption. Supportive care and medical management may be necessary to address liver inflammation and prevent further damage.
Causes and Risk Factors
Understanding the causes and risk factors of fatty liver disease is crucial for prevention and early intervention. Both NAFLD and AFLD share some common risk factors, but they also have distinct triggers.
Causes:
- NAFLD: The primary cause is metabolic dysfunction, including obesity, insulin resistance, and type 2 diabetes. Genetic predisposition and certain medications can also contribute.
- AFLD: The direct cause is excessive alcohol consumption, which overwhelms the liver’s ability to process and metabolize alcohol efficiently.
Risk Factors:
- Obesity: Excess body fat increases the risk of developing both NAFLD and AFLD.
- Type 2 Diabetes: Insulin resistance associated with diabetes is a significant risk factor for NAFLD.
- High Blood Pressure and High Cholesterol: These conditions can exacerbate liver fat accumulation and inflammation.
- Genetics: Genetic predisposition can influence the likelihood of developing NAFLD.
- Alcohol Consumption: For AFLD, the quantity and frequency of alcohol intake are crucial factors. Chronic heavy drinking is a significant risk factor.
- Medications: Some medications can contribute to liver fat accumulation and inflammation.
Preventive Measures:
- Healthy Lifestyle: Regular exercise, a balanced diet, and maintaining a healthy weight are key preventive strategies.
- Moderation of Alcohol Intake: Limiting alcohol consumption can prevent AFLD and mitigate its progression.
FDA Guidelines and Regulations on Fatty Liver Disease
Overview of FDA’s Role in Fatty Liver Disease
The U.S. Food and Drug Administration (FDA) plays a crucial role in managing fatty liver disease by regulating the approval of treatments, providing guidelines for diagnosis, and overseeing clinical research. The FDA’s responsibilities include ensuring the safety and efficacy of medications, issuing recommendations for healthcare providers, and supporting advancements in medical research.
Key Functions of the FDA:
- Drug Approval: The FDA evaluates and approves medications for the treatment of fatty liver disease based on clinical trial data that demonstrate safety and effectiveness.
- Guidance and Recommendations: The FDA issues guidelines for the diagnosis, management, and monitoring of fatty liver disease, helping healthcare providers deliver evidence-based care.
- Clinical Trials Oversight: The FDA monitors and approves clinical trials that explore new treatments and therapies, contributing to the development of innovative solutions for fatty liver disease.
FDA-Approved Medications and Treatments
The FDA has approved several treatments for fatty liver disease, particularly for its more severe forms such as non-alcoholic steatohepatitis (NASH). The goal of these medications is to reduce liver inflammation, improve liver function, and address underlying risk factors.
Current Approved Drugs
As of now, there are a few FDA-approved drugs specifically indicated for the treatment of fatty liver disease. These include:
- Pioglitazone (Actos): Originally developed for type 2 diabetes, pioglitazone has shown benefits in reducing liver fat and inflammation in patients with NASH.
- Vitamin E: High-dose vitamin E is sometimes used as an off-label treatment for NAFLD and NASH, particularly in non-diabetic patients, due to its antioxidant properties.
- Obeticholic Acid (Ocaliva): Approved for primary biliary cholangitis, obeticholic acid is also being investigated for its efficacy in treating NASH with fibrosis.
Note: The effectiveness of these treatments can vary, and their use should be tailored to individual patient needs and conditions. It’s important for patients to consult their healthcare providers about the best treatment options.
Emerging Therapies and Clinical Trials
Ongoing research and clinical trials are exploring new therapies for fatty liver disease. These emerging treatments aim to address the limitations of current medications and provide more effective options for patients.
- Anti-Fibrotic Agents: Drugs targeting liver fibrosis are being developed to halt or reverse liver scarring associated with advanced NASH.
- GLP-1 Receptor Agonists: Medications like semaglutide, used for type 2 diabetes, are showing promise in reducing liver fat and improving metabolic profiles in NASH patients.
- Gene and Cell Therapies: Innovative approaches, such as gene editing and stem cell therapy, are under investigation to address the underlying causes of fatty liver disease at a molecular level.
Clinical Trials: Numerous clinical trials are underway to evaluate the safety and efficacy of these new therapies. Participation in clinical trials offers patients access to cutting-edge treatments and contributes to the advancement of medical knowledge.
FDA Recommendations for Diagnosis and Monitoring
The FDA provides guidelines to help healthcare providers diagnose and monitor fatty liver disease effectively. These recommendations are based on the latest scientific evidence and aim to standardize care and improve patient outcomes.
Diagnosis:
- Imaging Techniques: The FDA recommends using non-invasive imaging techniques such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) to assess liver fat accumulation and detect liver damage.
- Biopsy: In cases where non-invasive methods are inconclusive, a liver biopsy may be recommended to confirm the diagnosis and evaluate the extent of liver inflammation and fibrosis.
Monitoring:
- Regular Check-Ups: Patients with fatty liver disease should undergo regular follow-up appointments to monitor disease progression, response to treatment, and liver function.
- Laboratory Tests: Routine blood tests to measure liver enzymes (e.g., ALT, AST), lipid levels, and other relevant biomarkers are essential for assessing the effectiveness of treatment and detecting potential complications.
- Lifestyle Assessment: Monitoring lifestyle factors such as diet, exercise, and weight changes is crucial for managing fatty liver disease and reducing associated risks.
Managing Fatty Liver Disease
Managing fatty liver disease effectively requires a multi-faceted approach that includes lifestyle changes, medical interventions, and regular monitoring. This comprehensive management strategy helps to slow disease progression, alleviate symptoms, and improve overall liver health.
Lifestyle Changes and Diet Recommendations

1. Healthy Diet:
- Balanced Nutrition: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. A Mediterranean diet, which emphasizes these components, has been shown to benefit liver health.
- Reduce Saturated and Trans Fats: Minimize intake of saturated fats (found in red meat and full-fat dairy products) and trans fats (found in processed foods and baked goods) to decrease liver fat accumulation.
- Limit Sugars and Refined Carbohydrates: Reduce consumption of sugary beverages, sweets, and refined carbohydrates like white bread and pastries, which can contribute to insulin resistance and worsen fatty liver disease.
2. Weight Management:
- Gradual Weight Loss: Achieving and maintaining a healthy weight is crucial. Aim for a gradual weight loss of 1-2 pounds per week, as rapid weight loss can exacerbate liver problems.
- Regular Physical Activity: Engage in regular exercise, such as brisk walking, jogging, or cycling, for at least 150 minutes per week. Exercise helps reduce liver fat, improve insulin sensitivity, and support overall health.
3. Alcohol Moderation:
- Limit Alcohol Intake: For those with alcoholic fatty liver disease (AFLD), abstaining from alcohol is essential. Even for non-alcoholic fatty liver disease (NAFLD), limiting alcohol consumption can reduce stress on the liver.
4. Smoking Cessation:
- Quit Smoking: Smoking exacerbates liver damage and increases the risk of liver-related complications. Seek support and resources to help quit smoking.
Medical Interventions and Therapies
1. Pharmacological Treatments:
- FDA-Approved Medications: As previously mentioned, medications like pioglitazone and vitamin E are used to manage NAFLD and NASH. Consult with a healthcare provider to determine the appropriate medication based on individual health conditions.
- Emerging Therapies: New treatments, including anti-fibrotic agents and GLP-1 receptor agonists, are being researched and may offer additional options for managing fatty liver disease.
2. Managing Comorbid Conditions:
- Diabetes Control: For patients with type 2 diabetes, tight glycemic control is crucial in managing NAFLD. Medications and lifestyle changes should be tailored to control blood sugar levels effectively.
- Cholesterol and Blood Pressure: Managing high cholesterol and hypertension through diet, medication, and lifestyle modifications can help reduce the risk of liver damage.
3. Surgical Options:
- Bariatric Surgery: In cases of severe obesity where lifestyle changes have been insufficient, bariatric surgery may be considered. This can lead to significant improvements in liver health, especially in individuals with NAFLD.
Monitoring and Follow-Up Care
1. Regular Medical Check-Ups:
- Scheduled Appointments: Regular follow-up visits with a healthcare provider are essential for monitoring liver health, assessing treatment effectiveness, and making necessary adjustments to the management plan.
2. Laboratory Tests:
- Liver Function Tests: Routine blood tests to measure liver enzymes (e.g., ALT, AST), bilirubin levels, and other indicators of liver function help track disease progression and response to treatment.
- Imaging Studies: Periodic imaging, such as ultrasound or MRI, can assess changes in liver fat content and detect any progression in liver fibrosis.
3. Patient Education:
- Self-Management: Educate patients on recognizing symptoms of worsening liver disease, understanding medication side effects, and adhering to lifestyle changes.
- Support Resources: Provide information on support groups, educational materials, and resources for further assistance with managing fatty liver disease.
4. Lifestyle Monitoring:
- Diet and Exercise Tracking: Encourage patients to keep a record of their diet, physical activity, and weight changes to help them stay on track with their management plan.
Innovations in Fatty Liver Disease Treatment
Innovations in the treatment of fatty liver disease are pushing the boundaries of conventional therapies and offering new hope for patients. Key areas of innovation include:
Gene Editing and Therapy: Advances in gene editing technologies, such as CRISPR, are being explored for their potential to correct genetic mutations and modulate gene expression related to fatty liver disease. These approaches could provide targeted treatments at the genetic level.
Cell-Based Therapies: Stem cell therapy and regenerative medicine are being investigated for their potential to repair liver damage and regenerate healthy liver tissue. These innovative treatments aim to restore liver function and reverse fibrosis.
Biomarker Development: Researchers are working on identifying new biomarkers that can provide more precise diagnostics, predict disease progression, and monitor treatment responses. Biomarkers could help in personalizing treatment plans and improving patient outcomes.
Non-Invasive Diagnostic Tools: New technologies are being developed to offer more accurate and less invasive methods for assessing liver fat and fibrosis. These tools could enhance early detection and monitoring without the need for liver biopsy.
Digital Health and Artificial Intelligence: The integration of digital health technologies and artificial intelligence (AI) is transforming the management of fatty liver disease. AI algorithms are being used to analyze complex data from imaging studies, laboratory tests, and patient records to improve diagnosis and treatment strategies.
Conclusion
Fatty liver disease presents a significant health challenge, characterized by the accumulation of excess fat in the liver that can lead to inflammation, fibrosis, and ultimately more severe liver conditions. Effective management of this condition requires a comprehensive approach that integrates lifestyle changes, medical interventions, and vigilant monitoring.
Recent advancements and ongoing research are bringing new hope for patients through the development of novel therapies and more effective treatment strategies. The FDA’s role in approving and regulating medications, guiding clinical practices, and supporting research is crucial in driving progress in the field.
Lifestyle modifications, such as adopting a healthy diet, engaging in regular physical activity, and managing comorbid conditions, remain foundational in the management of fatty liver disease. Meanwhile, the landscape of medical treatments is evolving with emerging drugs and therapies that target various aspects of the disease, from liver fat reduction to fibrosis reversal.
The future of fatty liver disease management looks promising with innovative research initiatives and clinical trials paving the way for breakthroughs. Emerging technologies, such as gene editing, cell-based therapies, and advanced diagnostic tools, are poised to revolutionize how we understand and treat this condition.
For patients and healthcare providers alike, staying informed about the latest research and treatment options is essential for navigating the complexities of fatty liver disease and improving patient outcomes. With continued advancements and a proactive approach to management, there is hope for more effective treatments and a better quality of life for those affected by fatty liver disease.
FAQs about FDA Fatty Liver Disease
What does the FDA do for fatty liver disease?
The FDA approves medications, provides guidelines for diagnosis and management, and oversees clinical trials for fatty liver disease.
Which FDA-approved drugs are available for fatty liver disease?
FDA-approved drugs for fatty liver disease include pioglitazone for NAFLD and obeticholic acid for NASH, with vitamin E used off-label for NAFLD.
Are there new treatments being explored for fatty liver disease?
Yes, new treatments include anti-fibrotic agents, GLP-1 receptor agonists, and gene or cell therapies, which are currently under investigation in clinical trials.
How does the FDA guide the diagnosis of fatty liver disease?
The FDA recommends non-invasive imaging techniques like ultrasound or MRI and, when necessary, liver biopsy to diagnose fatty liver disease.
What are FDA’s recommendations for monitoring fatty liver disease?
The FDA advises regular check-ups, liver function tests, imaging studies, and lifestyle assessments to monitor the disease’s progression and treatment efficacy.
How can I find information about clinical trials for fatty liver disease?
You can find information on ClinicalTrials.gov or by contacting research institutions and healthcare providers involved in fatty liver disease studies.